Abstract
Introduction
Arterial thromboses, such as ischemic stroke, peripheral vascular disease, myocardial infarction, are common complications among patients with myeloproliferative neoplasms (MPN). Reported incidence of thromboses ranges from 12%-39% in Polycythemia Vera (PV) and from 11%-25% in Essential Thrombocythemia (ET). Previous studies suggested that chronic hypoxia from living in higher elevation might be an independent prothrombotic risk factor. The goal of this study is to evaluate the frequency of thromboses and prothrombotic risk factors in patients with MPN at an elevation of 5000 feet above sea level and beyond.
Method
We selected 110 patients, who were diagnosed with MPN in University of New Mexico Comprehensive Cancer Center from 2001 to 2016. Ninety-four patients (85%) were living in Albuquerque metropolitan area with an elevation of 5312 feet above sea level and others were located in areas with an elevation of 6000 feet or higher in New Mexico. A retrospective chart review was conducted to identify clinical and molecular risk factors for both arterial and venous thromboses. The mutation analyses for Janus Kinase 2 (JAK2), myeloproliferative leukemia (MPL) gene and calreticulin (CALR) gene were performed by polymerase chain reaction (PCR). Contingency table and logistic regression methods were applied to analyze and compare the distribution of the prothrombotic risk factors between the patients with and without thrombosis.
Results
In this study, 62 patients (56%) were diagnosed with ET, 33 patients (30%) with PV, and 15 patients (14%) with primary myelofibrosis (PMF). Sixty-six patients (60%) were females. Thirty-six patients (33%) experienced either arterial or venous thromboses. A significant number of thrombotic events (30 out of 36) were either ischemic stroke or myocardial infarction. The patients with thromboses were slightly older with mean age of 63 years old compared to 61 years old for the patients without thrombosis. The patients with thromboses were predominantly males (21/36, 58%) while the majority of patients without thromboses were females (51/74, 69%) with p= 0.011. Nineteen (53%) patients with thromboses had ET; however a higher proportion of patients with PV (15/33, 45%) developed thromboses compared to ET or PMF (13% or 31% respectively, p= 0.078). In addition, a significant number of patients (26/36, 76%) with thromboses have JAK2 mutations (p= 0.066) while only 2 patients (6%) have CALR gene mutation and 3 patients (9%) have MPL gene mutation. Although not statistically significant, JAK2 mutation was strongly associated with more thrombotic events than CALR mutation.
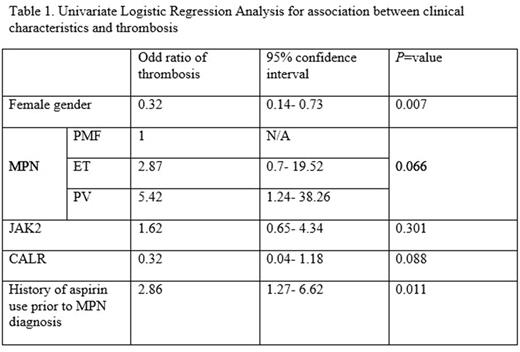
In univariate logistic regression analysis, gender and history of aspirin use prior to MPN diagnosis are the only clinical characteristics that are significantly associated with increased thrombotic events. History of aspirin use was significantly associated with increased thromboses with an odd ratio of 2.86 (p=0.011). Female gender was associated with decreased thrombotic events with an odd ratio of 0.32 (p=0.006). Patients with PV showed a 5.4-fold increase and patients with ET have a 2.9-fold increase in odds for thrombosis compared to patients with PMF (p=0.066). There was no significant difference between patients with and without thromboses, regarding other clinical characteristics such as age, leukocytosis, diabetes, hypertension, hyperlipidemia, obesity and smoking.
Conclusion
The increased frequency of arterial thromboses was observed among patients with MPN, significantly higher than previously reported studies performed at sea level. This strongly suggests the role of mild to moderate hypoxia as a contributing prothrombotic risk factor for MPN. The role of chronic hypoxia and its influence in thrombotic events in MPN need to be further evaluated in prospective studies.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal